Published on
Future-Proofing Medical Education: Transitioning to a Competency Model

Just as the music and publishing industries have adapted to changing societal norms, lifestyles and emerging technology, so must health care and medical education.
The health care delivery environment is rapidly changing and the need for innovation is immediately apparent. With cutting-edge technology, portable health care data, global online collaboration, dramatic new scientific discoveries, precision medicine and comprehensive health care reform, we must completely transform medical education to improve health care and health outcomes for society.
In response to these market transformations, in the fall of 2014, the OHSU School of Medicine implemented YOUR M.D., a radical faculty-driven transformation of traditional medical school curriculum that integrates diverse perspectives with scientific research on learning. This was a large development process that involved the extensive input of many community members including patients, providers, students, alumni and administrators, but the outcome is a program designed to help ensure future physicians are ready to thrive in this complex health care delivery environment.
The goal of this initiative is simple: to effectively prepare medical students for their residency training and professional practices in order to meet the needs of society. Graduates will be equipped to enter the health care landscape as systems thinkers and improvement specialists, ready to provide care that is patient-centered, coordinated, adaptable to change, and always improving. They will be skilled master adaptive learners who understand that improving the system in which we work is an integral part of the work physicians must do every day.
Answering the Challenges of Tradition
Traditionally, medical schools have been structured in a “2+2” model that is time-fixed: two years of basic science learning taught primarily in a classroom setting, followed by another two years of hospital-based clinical rotations. Under this system, students typically spent over half of their time watching lectures, memorizing and reading with a focus on acquiring basic scientific knowledge. It wasn’t until the clinical years that these students learned the patient-care and procedure skills considered essential to becoming a physician. While there is no question that scientific knowledge, patient care and procedure skills are absolutely critical to medical education, what is missing in this traditional system is attention to other, equally important elements of doctoring, including communication, collaboration, teamwork, critical-thinking, quality improvement, efficient use of system resources and professionalism.
Today’s physicians need to know a lot, but discovering answers to new questions, embracing a team approach, and integrating health care delivery science—things like patient safety, clinical informatics and population health—into daily practice are equally important lifelong skills.
To help resolve this challenge, the new Foundations of Medicine portion of the YOUR M.D. curriculum [Figure 1] utilizes a case-based teaching method, which “spirals” instructional content in the curriculum across a defined set of threads. This fully integrated curriculum allows students to learn in context, rather than compartmentalize issues and ideas into a single course in isolated areas. Following this coursework, students then have the ability to practice—and be assessed on—their learned skills in a safe environment in a state-of-the-art simulation facility utilizing standardized patients (i.e., actors) and other high-fidelity simulation methods.
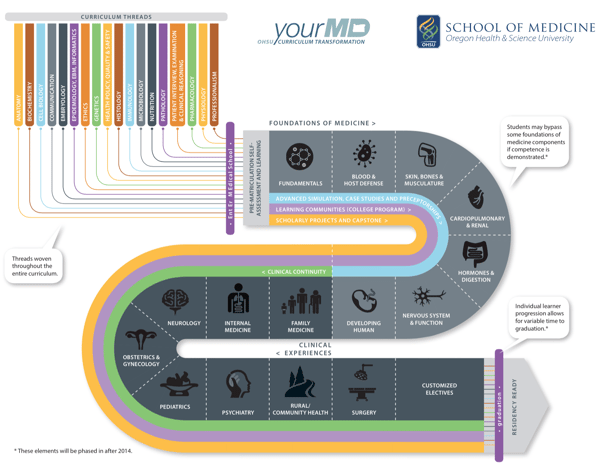
Once the Foundational phase of the curriculum is completed, each student enters a flexible and individualized clinical experience phase of the curriculum. This includes core experiences in traditional disciplines such as pediatrics, surgery and psychiatry, but also a wide range of elective clinical experiences such as anesthesiology, emergency medicine and dermatology, that have historically not been available until the fourth year of traditional medical school. Additionally, all students complete a rural clinical experience offered in a variety of specialties, as well as a new continuity clinical experience. These opportunities allow students more in-depth learning across disciplines and patient settings. Intersessions and Scholarly Projects help students fully integrate foundational science with clinical and health care delivery science in their later years of training.
Finally, YOUR M.D. provides feedback to students each week about their academic performance, which, along with the help of their personal academic coach, is analyzed to help guide their individual improvement plan. This feedback process is important, because to obtain a degree through YOUR M.D., students must demonstrate entrustment for the 43 OHSU-defined M.D. competencies, as well as the nationally defined 13 entrustable professional activities (EPAs) for entering residency.
With this newly transformed curriculum, OHSU will produce “residency-ready” graduates who are entrusted to enter their residency training by demonstrating competencies using many assessments in a variety of clinical and non-clinical contexts. Once fully implemented, our competency-based educational model will ensure that students will graduate when they are ready to move to the next phase of their medical education. For some, this will mean the opportunity to accelerate through the program and graduate in less than the traditional four years of training. This helps society by increasing the pool of qualified residents at a faster pace, while also providing the opportunity for students to finish their M.D. program with lower indebtedness.
Adding Polish to the Process
As with any transformational innovation, the process of changing our curriculum has not been without challenge.
We deliberately implemented our new curriculum on a fast timeline and—throughout our first year execution—relied heavily on frequent student, staff and faculty feedback to determine opportunities for improvement and program refinement. For example, we adjusted the weekly schedule to allow students more daily variety of large and small group learning activities in combination with science and clinical skill laboratories. We also created processes to assist faculty instructors in utilizing the advanced technology available in the learning studio, as well as help in incorporating more active-learning teaching methodologies rather than simply lecturing.
Key insights were incorporated into the curriculum delivery prior to the start of our 2015-16 academic year, and much like the mentality we are instilling in our M.D. students, the OHSU faculty is committed to evolving aspects of our program to achieve desired outcomes, all with a continual improvement mindset.
Producing the Future
Overall, a competency-based approach to medical education will create master adaptive learners who are accustomed to frequent self-assessment, use and interpretation of performance data to guide continual improvement. There has never been a more exciting time in medical education, and it is compelling to think about how our forthcoming physician graduates will be primed to become the change-agents for advancing the future of healthcare across the nation.
Author Perspective: Administrator



