Published on
Medical MOOCs: Lessons Learned from the Trenches of Medical Education

Massive open online courses (MOOCs) offer high-quality content from world-class universities to anyone with access to the worldwide web for free. Since their inception in 2012, much has been written in the popular press and by academicians opining in editorials, blogs and scholarly journals on the value of MOOCs and their likely impact on the future of higher education, even medical education. For their part, thought-leaders in academic medicine are already predicting the transformative impact of MOOCs across the continuum of education in the health professions. For example, Mehta et al. envisioned MOOCs as a key facilitator of competency-based, learner-centered medical education that can better meet the needs of societies and their changing healthcare systems.[1] Prober and Khan argued that several key strategic factors are driving the need to “reimagine” medical education where online learning would facilitate evidence-based, flipped-classroom teaching and cost-efficient, cooperative curriculum sharing across schools of medicine.[2]
Many of us in medical education agree with these fundamentals and recognize that MOOCs (and other eLearning innovations) convey the potential to radically transform both the means and costs of education in the health professions for post-baccalaureate students, residents, fellows and even licensed healthcare professionals.[3] My purpose here is not to advocate for such transformation, although most of my campus-based students would surely welcome it. Rather, my goal is simply to share five lessons that I am learning from the trenches of medical education through my efforts to create a blended learning environment for the development of future healthcare professionals in the neurological sciences.
In my case, the centerpiece of this learning environment is a MOOC called Medical Neuroscience that I created and launched on the Coursera platform in January 2013. This was the first medical MOOC designed to be similar in scope, content and academic rigor to what first-year medical or physical therapy students would experience in their preclinical, biomedical science curriculum. Medical Neuroscience features 45 hours of video tutorials accompanied by written study guides that are organized into six units of content: human neuroanatomy, neural signaling, sensory systems, motor systems, brain development and cognition. Student learning is supported by a course wiki with links to additional free online resources, a robust discussion forum equipped with user-voted posts, a team of volunteer community teaching assistants who moderate student discussions, and periodic online hangouts for real-time, face-to-face conversation. The assessment strategy includes six unit quizzes, two peer-assessed assignments, a functional neuroanatomy exam, and a comprehensive case-based final exam.
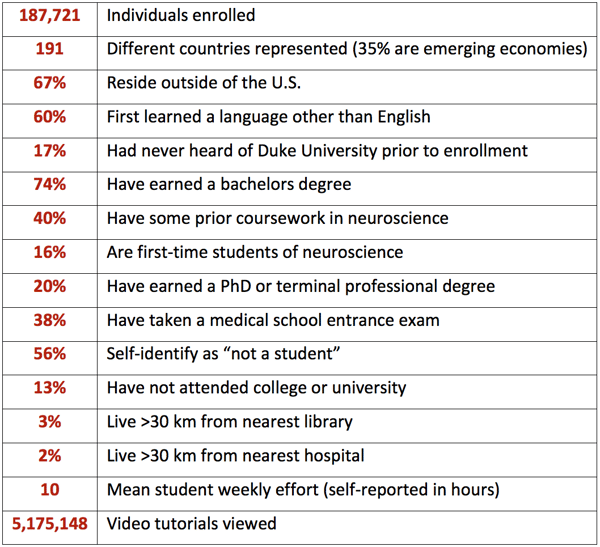
As my students have attested in forum posts and external blogs, Medical Neuroscience is a serious course. In fact, it has long been the toughest MOOC in the Coursera catalog, as reflected by the depth and breadth of instruction, the expected weekly workload (16-20 hours), and the duration of the course (12 weeks). Despite these challenges, or perhaps because of them, over 100,000 individuals from all walks of life and all corners of the globe have engaged content across three runs of this course and one run of a shorter derivative course (Foundational Neuroscience for Perception and Action). The table below provides a profile of the experience to date.
At the Duke University School of Medicine and the Duke-NUS Graduate Medical School (Singapore), Medical Neuroscience is framed by a team-based learning curriculum for real-time, collaborative learning in a campus-based course for first-year medical students that I co-direct called “Brain and Behavior.”[5] Thus, the blended learning environment that I’ve been describing comprises a MOOC for didactic instruction and a flipped-classroom course for collaborative learning, hands-on application (human brain dissection), problem solving (clinical case analysis), and professional formation.
So here’s what I’m learning now that I am three years into this venture.
Lesson 1: Align with the preferences of the learners
If MOOCs are to realize their potential impact on the education of future healthcare professionals, they must align with the needs and preferences of our learners in several important respects. Nearly all of our entry-level learners in the healthcare professionals are digital natives, being fully competent in the means for accessing knowledge (on any subject) at anytime from anywhere for any purpose. If Prensky was correct when he eloquently described these learners and the challenges facing their digital immigrant educators, MOOCs may very well provide a culturally transformative means for acquiring knowledge and developing the scholarly skills necessary for real-life application and lifelong learning—skills that are essential for competent provision of evidence-base care in the health professions.[6]
As a digital immigrant myself (and one who barely cleared digital customs), I am finding my way in this cross-cultural landscape being guided by what I am trying to learn from cognitive scientists studying online teaching and learning (most notably, Richard E. Mayer, Professor of Psychology at the University of California, Santa Barbara). Consequently, I have endeavored to create modular content, packaged in brief video tutorials (average duration at 1X = 13 minutes) that minimize the burden of cognitive overload and distraction while maximizing the potential for authentic—albeit mediated—connection from teacher to student. Which leads me to the next and perhaps most important lesson.
Lesson 2. Teach through the medium.
From the inception of my MOOC, I’ve tried to give students the experience of a private tutorial—as if they have come to my office for help or scheduled a meet-up somewhere on campus. To achieve this aim, I never record a live lecture just so that it can be repurposed for the MOOC. After all, who wants to be a fly on the wall in somebody else’s lecture hall?
Instead, I teach directly to a camera being as mindful as possible of the learners on the other side of the medium. On their end, students see my face and enough of my upper body to capture my gestures throughout most of each video tutorial, with a variety of illustrations, graphics, photographs and video clips filling the rest of the screen. I have also avoided “green screen” (weather-person) videographic techniques, because I want students to see me in context (simulating the private tutorial experience). So behind me in the picture-in-picture window, students see my laboratory, my academic office, my living room, my backyard, the Duke Forest, and enough of campus to get a feel for the general environs of Duke University (in one video, they even see me rattle home a three-point basketball shot on the floor of famed Cameron Indoor Stadium). In post-course surveys of my campus-based medical students, 91 percent considered the video tutorials from Medical Neuroscience to be “extremely useful” (top tier) for their learning, while only 19 percent of students in the year prior to the introduction of this MOOC rated lecture-captured videos (the medical school’s standard at the time) in this tier.
The point of all of this is not personal vanity, or at least I’d like to think so. The point is to make learning personal. I never would have believed this before creating this MOOC, but students online truly value relationship just as much as content—even virtual relationship that is one-sided and mediated by screens large and small (a significant fraction of my students regularly view my tutorials on handheld devices).
Lesson 3: Disruption runs deep
Let’s face it: MOOCs are a disruptive innovation. Many of my colleagues have little interest in reimagining medical education, some actively oppose it, and there are more than a few who feel downright threatened by talk of doing so. But like it or not, our medical learners have long since embraced the learning strategies predicated in the fundamentals outlined by Prober and Khan.[7] For example, prior to implementation of my current blended learning environment I have seen students laboring over outsourced content (often of unknown provenance) and disarticulated instructional media (often lectures captured in somebody else’s amphitheater). These unsanctioned materials amounted to an underground curriculum that students often seemed to value for no better reason than they were obtained through peer-to-peer networks. To be fair, there certainly are excellent resources created by learners across the continuum of medical education and shared (usually freely) for the benefit of more junior peers. These are exactly the sort of resources that should be liberating faculty educators to do what we do best: guide our students into the application of biomedical knowledge, the development of clinical skills, and the maturation of professional values for practice and lifelong learning. I would respectfully encourage my colleagues to consider medical MOOCs in this same light.
But medical MOOCs can cast a dark shadow. While I have sought to optimize the efficacy and efficiency of the blended learning environment for my own campus-based students, I do worry that by making my MOOC freely available to anyone, it has become someone else’s underground curriculum for biomedical education. This is not just a worry. I have received numerous emails from medical students from around the world who have attested to the essential value of Medical Neuroscience for their own progression through their “above ground” curriculum. My apologies to those medical educators with these students in their courses; I certainly do not mean to add noise to the learning experiences that you are skillfully crafting for your students.
Lesson 4: Diversity matters
In recent years, we’ve seen a welcome and long-overdue focus on the value of diversity in medical education as medical schools aspire to address the urgent need to generate a work force in the healthcare professions that reflects the communities it serves with empathy, competency and humility. I’m proud of the efforts we have made at the Duke University School of Medicine to make this more than an aspiration. As my Duke Medicine colleague, Dr. Damon Tweedy, recently wrote, “Over time, such efforts could produce a greater cohort of doctors who are better prepared to relate to the patients who need them the most.”[8]
In our blended learning environment built around the principles and practices of team-based learning, diversity is our greatest strength. At Duke, we engineer our student teams to maximize their diversity across every dimension of academic, biometric, cultural, and socioeconomic status that we can identify. But even these distributions pale in comparison to the diversity inherent in a moderately-sized MOOC, such as Medical Neuroscience (see table). One additional dimension of diversity worth noting that I completely underestimated is age. My demographic target was the twenty-somethings who constitute the largest cohort in medical schools. As it has turned out, less than 60 percent of Medical Neuroscience students are in this age range. In fact, 7 percent of the students in my most recent run are older than 65.
At no time in the MOOC is the power of diversity more evident than when we conduct our periodic live hangouts. These videoconferences give anyone in the course opportunity to make themselves visible as they put face and voice to their unique contributions. I am profoundly grateful for their willingness to do so at all hours of the day and night wherever they may be.
Lesson 5: Never underestimate the passion and creativity of the learner
If my lesson #2 above is most important, then lesson #5, with which I close, is certainly the most powerful lesson learned. It is the lesson that has most impacted my approach to on-campus teaching.
As I began this MOOC, I must admit that I rather cynically supposed that people would NOT value what was offered for free. I was arrogant and naïve. I failed to appreciate how much of themselves people were willing to invest in their learning; they were paying with their time, attention, effort and creative energy. Thankfully, it did not take me long to correct my erroneous supposition and begin considering how I might align learning opportunities with the creative energies of the students. For instance, the peer-assessed assignments in Medical Neuroscience require constructing original, visual representations of brain structure and function, with an emphasis on the surface anatomy of the human brain and the neural systems that mediate the experiences of touch and pain. It has been sheer delight to survey the gallery on the course site of the most accurate and impactful submissions, as determined by the students themselves. We’ve seen everything from the skilled renderings of individuals with serious artistic talent to constructs made from found items including produce, holiday decorations, and human body parts (all very much attached and fully animated!).
These creative works have inspired me to go deeper into social spaces to provide means for creative expression of student learning. In our most recent course, we used our Twitter account to challenge students to share photographs of their own experience of the course, unexpected images of neuroscience encountered in everyday life, and even original haikus, limericks and other poetic forms. These challenges have been great fun for students and course staff alike. But they are also great means for mobilizing and synthesizing knowledge in creative ways that I have now begun to utilize in my on-campus teaching. More significantly, the passion and creativity of the online learning community in my course have fundamentally reshaped my understanding of the learner. I am intentionally and strategically viewing my students online and on-campus as collaborators in the joy of discovery and learning. I can think of no greater privilege for an educator in any discipline.
– – – –
References
[1] Mehta, N.B., Hull, A.L., Young, J.B., Stoller, J.K. (2013) Just imagine: new paradigms for medical education. Acad. Med. 88:1418–1423.
[2] Prober, C.G. and Khan, S. (2013) Medical education reimagined: a call to action. Acad. Med. 88:1407–1410.
[3] Sharma, N., Doherty, I., Harbutt, D. (2014) MOOCs and SMOCs: changing the face of medical education? Perspect. Med. Educ. 2014 Jan 30.
[4] Data compiled on June 15, 2015.
[5] Kamei, R.K., Cook, S., Puthucheary, J., Starmer, C.F. (2012) 21st century learning in medicine: traditional teaching versus team-based learning. Med. Sci. Educ. 22:57-64.
[6] Prensky, M. (2001) Digital natives, digital immigrants. On the Horizon 9:1–6.
[7] Prober and Khan (2013)
[8] Damon Tweedy, “The Case for Black Doctors,” The New York Times, May 15, 2015. Accessed at http://www.nytimes.com/2015/05/17/opinion/sunday/the-case-for-black-doctors.html?mwrsm=Email&_r=0



